925
Views & Citations10
Likes & Shares
Between July 2016 to March 2017, I got involved as a Senior Medical
Doctor and Technical Support Officer to Northern and Eastern Shan State for the
PEPFAR Project of USAID with PSI (Population Service International) and
Malteser International. I was responsible for prevention and treatment of
infectious diseases especially in HIV/AIDS and Harm Reduction of Narcotic drug
users in Shan State. This was professionally very challenging and actively
involved the management of multi-faceted on health threats, including HIV, HCV
and Blood borne diseases prevention in Lashio and Muse, then Maternal health,
Child health and Nutrition Program in Eastern Shan State for Malteser
International Organization and Data collection in disease prevalence of
Malaria, Dengue Hemorrhage Fever, Diarrhea, Nutritional Deficiency and
Environment Hazards. It was personally challenging, with the requirement to
travel extensively and negotiate with wide range of individuals and different
sectors while the situation was still under the reconciliation for peace and
truce.
Keywords: Myanmar, Shan
State, Healthcare, Facility, Infectious diseases
MALARIA
The assessment of the
malaria risk throughout the mission was extremely variable Information about
malaria epidemiology in the four special regions is very sparse. For example,
malaria in Kyaing Tong Eastern Shan State (Predominantly Plasmodium falciparum and P.
vivax are the major malaria infections) was characterized by a number of
variables including irrigation, temperature, attitude and season. The higher
prevalence was noticed in children in this region [1]. The proportion of P. vivax to P. falciparum infection was relatively more noticeable than that of
malaria cases recorded in clinics and hospitals. That seems the prevalence of P. vivax infection may be underestimated
[2]. Historically most frequent out breaks were documented in year 1998 and
1999. During 1991-2004, highest frequencies of malaria epidemics occurred in
Shan States mainly due to new settlement (Wa region), changing agricultural
practices (Kokant area), epidemic prone villages (Southern Shan State) and some
development projects constructed at endemic areas. Most of the epidemics in
Rakhine across Mayu Hilly Region [3]. Observation of treatment behavior for
malaria patients in Namkham, Northern Shan State study (done by Dr. Khin Maung
Wynn, State Health Director, Kayah; previous malariologist) pointed out that
self-treatment (39.3%) is usually common (154 patients out of 392). Treatment
results by self-medication were 227% of cases cured and 37.7% of cases became
worse. Similar result is seen in treatment given by drug sellers. It implies
that we need to educate the community regarding the danger of self-treatment
and treatment given by non-health personnel. It also needs to educate important
of early diagnosis and appropriate treatment according to laboratory results
for adherence of new antimalarial treatment policy [4]. The autonomous and
insurgent regions in northern Myanmar are near the Yunnan Province, China,
whereas many malaria cases are probably imported from Myanmar though most are
still undetected due to illegal cross-border issue [5]. Behavior of illegal
immigrant crossing the border was considered as high risk for malaria control
in the border countries [6]. The cross-border cooperation mechanism in the
border area should be further strengthened to share the epidemiological data
about malaria, support technical assistance and conduct joint malaria control
or elimination activities [7-9]. Our Team did data collection about prevalence
and made rapid diagnostic for clinical treatment and made decision about the
strategies based on current issue of health threats along with local public
health department.
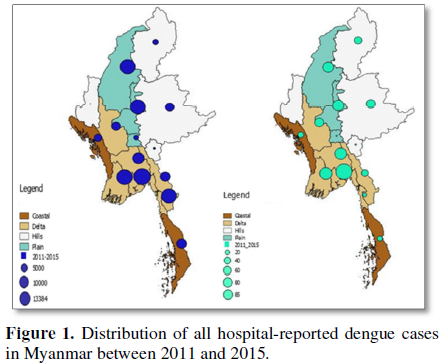
DENGUE HEMORRHAGIC FEVER
Between 1955 to 1959,
905 cases were recorded globally. In Myanmar, there were just over 6,000 DHF
cases between 1974 and 1976. More than 40,000 cases have been detected across
the country since 1976 to 2015. The largest number of cases happened in 2007,
2011, 2013 and 2015 but every 2 or 3 years the country has DHF epidemic usually
breaks out especially in Monsoon Season. More than 8,200 people of DHF victim
suffering from dengue shock syndrome and that the death toll reached 40 was
announced by Public Head Department according to recent epidemic data [10]. The
Shan state has seen relatively lower cases (970) than Mandalay region where has
the most cases (1268), followed by Yangon (1177) and 832 in Ayeyawady Region.
From 1976 to 2015, some 40,000 cases were occurred across the country [11]. The
nationwide report of the occurrence of DHF including Shan Stet is shown in Figures 1A and 1B. Since Shan State is
hilly region and most villages and towns are in very hard to reach areas, there
is difficult to access public transportation to hospital where are very far
away from villages and where has also shortage of medical staffs and equipment.
DIARRHEA
According to the
latest WHO data published in May 2014 Diarrheal diseases Deaths in Myanmar
reached 11,443 or 2.88% of total deaths. The age adjusted Death Rate is 25.64
per 100,000 of population ranks Myanmar #51 in the world. Diarrhea is a common
childhood illness in Myanmar and rotavirus is the single most important
etiological agent of diarrhea. Surveillance for rotavirus diarrhea in children
<5 years of age was conducted [12]. Due to the difficulties of getting safe
and clean water in Hilly Shan State, the most common illnesses here are
diarrhea, typhoid and skin infections due to a lack of clean water and personal
hygiene. Children are particularly vulnerable. The main direct causes of death
among children under five continue to be diarrhea (50% of impact morbidity in
Shan State), acute respiratory infection and malaria, exacerbated by underlying
malnutrition, which contributes to around 50% of these deaths, by UNICEF
consultant, Dr. Phone Myint [13].
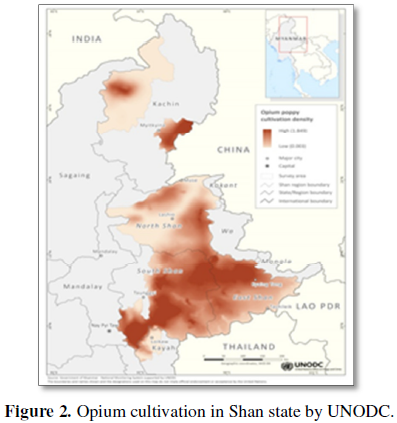
NARCOTIC ABUSE
Enhancing resilience to opium poppy cultivation in Shan State is still challenges implication for Alternative Development, Peace and Stability is dedicated to Shan State, highlighting reasons farmers engage in the opium economy, as well as some implications for Myanmar's ongoing peace process. A total of 591 villages in 39 opium poppy growing townships in Shan State were surveyed according to United Nations Office on Drugs and Crime (UNODC) report and the findings show that while many factors affect farmers' decisions regarding whether or not to cultivate opium poppy-including the condition of infrastructure and access to markets for other goods-governance and security considerations are significant factors. On average, round about two third of government controlled poppy villages are fewer than non-opium poppy villages (88%). At the same time, more opium producing villages have the perception of being "unsafe" or "very unsafe" (11%) than in non-opium poppy villages (2%). Most hazardous of narcotic abuse people are usually in mineral rich area such as Phar khant, Kachin state and Mogok. Death toll has soared from drug overdose and detrimental intravenous injection of poppy leading to death in these areas [14]. The Discussion of this issue is beyond the scope of my observation and it has been associated with national and global problem of drug and regional safety. The report detailing where opium cultivation in Shan State by UNODC is shown in Figure 2.
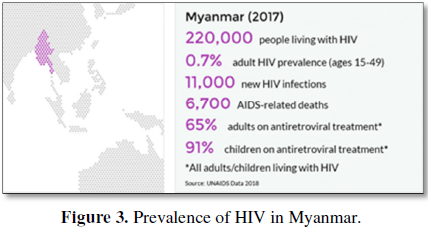
HIV/AIDS
Over 80% of injecting drug users in Northern Shan State, most of them who inject heroin, were found HIV infected and many of them have died. The Update on HIV in Myanmar in October 2004 by Jamie Uhrig, a researcher who had worked in Myanmar, called the rising prevalence of the epidemic as "The Crisis in Shan State.” According to his paper, over 80% of injecting drug users (IDUs) in Lashio, the vast majority of heroin user, were found HIV infected and many of them have died. However, HIV prevention programs have been disrupted by crackdowns on sex work and human trafficking and led to greater vulnerability of sex workers to HIV. 1.31% of all adults in Myanmar are estimated to be living with HIV in Myanmar, according to the National AIDS Program's official estimate. Far Eastern Economic Review, 15 July, reported that 5% of the 7 million people living with HIV/AIDS in Asia-Pacific Region are in Burma, while 61% are in India, 13% in China, 11% in Thailand and 10% in other countries. Elimination of mother-to-child transmission of HIV is a key component of the global response to HIV for young children. Steady expansion of HIV testing, particularly of pregnant women and provision of the most effective antiretroviral treatment (ART) offers hope that mother-to-child transmission can be virtually eliminated in low-and middle-income countries as well. The Myanmar National Strategic Plan on AIDS 2011-2015 includes prevention of mother-to-child transmission (PMTCT) as a priority and various related indicators are regularly monitored. Among those reached by the public health system, less than 60% of pregnant women across Shan are likely to be tested for HIV and receive the test result. Whether identified retro virus positive pregnant women in the State receive ART for PMTCT varies considerably between Shan North and South. And to a lesser extent, so does the probability of an infant born to an HIV-positive woman being tested for HIV within the prescribed 2 months after birth, which is as low as 21% in Shan North [15]. The national data of HIV condition in Myanmar is shown in Figure 3.
ENVIRONMENT HAZARD
In such a large region and diverse region, environment hazards included occupational hazards in Mining in Mong Yong and Mong La, dust, smoke and hypothermia (Particularly in Lashio and Kuk Khai). This required education, monitoring and protective equipment as appropriate. Quality data on the most salient child protection issues in Myanmar, such as children living in out-of-home residential care, children living and working on the street and children in hazardous forms of work, is currently unavailable. It is expected that with the population census and Demographic Health Survey in 2014-2015, relevant data will be collected and analyzed.
NUTRITION AND VITAMIN DEFICIENCY
Good nutrition is a
cornerstone for survival, health and development. Well-nourished children
perform better in school, grow into healthy adults and in turn give their
children a better start in life. Given the optimum start in life, all children
have the potential to develop within the same range of height and weight. Since
majority of terrain in Shan State is hilly and sloping region, the agriculture
and cultivation is difficult for them to plant nourished cultivation and they
are habitual in poppy planting rather than crops. We recognized that most
children and adolescent are deficient in vitamin (A, D, E and B complex) and
Iodine in Eastern Shan region. In Northern Shan State, the prevalence of
stunting (or low height-for-age) is alarmingly high with as many as 47% of
children being stunted [16-18]. Stunting is a con-sequence of chronic malnutrition
and can have irreversible damage on brain development. If not addressed in the
first two years of life, stunting diminishes the ability of children to learn
and earn throughout their lives.
CHILD HEALTH
Children have basic
needs, such as adequate nutrition and healthcare that if unmet could result in
long-term consequences including limitations on their physical and cognitive
development and consequently wellbeing in adulthood. Their experience of
poverty is multidimensional and deprivation in any of the key dimensions (i.e.,
nutrition, health, education, care and protection, water, sanitation and
income) compromises their wellbeing. Sizeable proportion of children in Shan
continue to have some of their most basic needs unmet, with a much greater extent
of deprivation in Shan North and Shan East compared to Shan South across a
number of indicators. According to Myanmar Public Health conference 2016, only
48% of births are registered in Shan North and 46% of the population is living
below the poverty line in Shan East. The Multiple Indicator Cluster Survey
(MICS) stated that the proportion of households that do not have access to
improved sanitation in Shan State ranges from 8% in Shan East to 32% in Shan
North. And open defecation rates are higher in Shan East and Shan North (3%
each) compared to Shan South (0.2%). The 2011 Survey on Water and Sanitation by
Ministry of Health revealed that the situation may actually be much worse,
especially in some areas. For example, about 52% of households were not using
improved latrines in Kutkai Township (Shan North). Improved sanitation can
reduce diarrheal disease by more than a third and can significantly lessen the
adverse health impacts of other disorders responsible for death and disease
among millions of children. Investment in hygiene promotion, sanitation and
water services is also among the most cost-effective ways of reducing child
mortality.
PERSONAL PERSPECTIVES ON DUTIES AND RESPONSIBILITIES
The multi-faceted
nature of the role was continually challenging and the dynamic situation meant
that nothing could be assumed. This required extensive travelling around the
region to develop and maintain situational awareness of health threats and
health support arrangements. The major challenges of changing health threats
are that there are a lot of them and they all require time and effort to manage
and mitigate. As many of them involve behavioral modification or training,
there is an opportunity cost involved, such that increasing the time for one
threat then reduces the effectiveness of training for other threats. In
addition, there is then a challenge in how this risk management process can be
effectively communicated to a non-medical command structure which required an
understanding of how the community team works. Fortunately, we had worked
together harmonically in trip to villages and remote areas and then well
collaborated with Government Regional Head and leaders of Autonomous Region for
Health Care improvement while there was still problem of reconciliation between
the groups in the regional peace and safety.
DISCUSSION
Myanmar health care
system evolves with changing political and administrative system and relative
roles played by the key providers are also changing although the Ministry of
Health remains the major provider of comprehensive health care. This review
briefly describes the recent situations of various aspects of healthcare in
Shan State, Myanmar, based on the most up-to-date data sources. The statically
relevant of the epidemiological data mentioned in this brief review lightens
the situation of health care stratus that is coincided with my experiences on
this mission. Although the health conditions in Myanmar have been improving as
exemplified by MDGs, there is a serious lack of facilities and healthcare
professionals. A new attempt to introduce a health insurance is expected to
further improve the conditions. Myanmar is now in transitional period of new
born democracy that is facing many challenges in different sectors including
health care system. Thus, national and international support is needed for
successful improvement in Myanmar. The present review article has shown the
experience of my mission with international organization and discussed bout the
heath care situation in Eastern Shan State.
CONCLUSION
To be an effective Medical Doctor, Technical Support Officer and Coordinator for a mission, a wide range of skills and capabilities are required, both professional and personal. Professional requirements include a broad range of medical care and practices, including tropical medicine, travel medicine, occupational medicine, public health and medical admiration, particularly as they apply to organization setting. While it is one thing to have knowledge in areas such as tropical and travel medicine, it is another thing to apply this in a dynamic programmatic setting. Effective risk management is vital to the effective performance of the Medical Doctor role, drawing all these elements together. Personal requirements include the ability to provide leadership to more junior health staff (even if they do not report to you directly), communication skills (especially with command and staff officers and other co-workers, the ability to be an effective team player, most importantly a good communication and friendly personality.
ACKNOWLEDGEMENT
I would like to thank
to co-workers of the mission, regional state holders and organizations.
1. Ru-bo W, Jun Z, Qing-Feng Z (2014) Malaria
baseline survey in four special regions of northern Myanmar near China: A
cross-sectional study. Malar J 13: 302.
2. Cui LW, Yan GY, Sattabongkot J, Cao YM, Chen
B, et al. (2012) Malaria in the Greater Mekong sub region: Heterogeneity and
complexity. Acta Trop 121: 227-239.
3. Zhou SS, Wang Y, Tang LH (2009) Malaria situation
in the People’s Republic of China in 2008 (in Chinese). Chin J Parasitol
Parasit Dis 27: 193-195.
4. Li JQ, Yang L (2009) Epidemic and control
situation of malaria in Baoshan city in 2008 (in Chinese). Parasitoses Infect
Dis 7:131-134.
5. Tipmontree R, Fungladda W, Kaewkungwal J,
Tempongko MA, Schelp FP (2009) Migrants and malaria risk factors: A study of
the Thai-Myanmar border. Southeast Asian J Trop Med Public Health 40:
1148-1157.
6. Pongvongsa T, Ha H, Thanh L, Marchand RP,
Nonaka D, et al. (2012) Joint malaria surveys lead towards improved
cross-border cooperation between Savannakhet province, Laos and Quang Tri
province Vietnam. Malar J 11: 262.
7. Chen GW, Zhao JY, Zhao XT, Zhao HY, Sun WJ,
et al. (2007) Investigation on the impact of joint cross-border malaria control
in Cangyuan county, Yunnan province, China (in Chinese). Parasitoses Infect Dis
5: 80-81.
8. Richards AK, Banek K, Mullany LC, Lee CI,
Smith L, et al. (2009) Cross-border malaria control for internally displaced
persons: Observational results from a pilot programme in eastern Burma/Myanmar.
Trop Med Int Health 14: 512-521.
9. http://www.traveldoctor.com.au/Article/Alerts/Africa/Dengue-hemorrhagic-fever-in-Myanmar
10. Herriman R (2016) Myanmar dengue case tally
tops 8,000.
11. Moe K (2005) Hospital-based surveillance for
rotavirus diarrhea in children in Yangon, Myanmar. J Infect Dis 1: 111-113.
12. Shwe Yee SM (2012) Myanmar's child mortality
still highest in region. UNICEF, Myanmar Time.
13. UNODC (2017) Opium cultivation in Shan State
is concentrated in areas with poor security. Myanmar Survey.
14. Myanmar National AIDS Programme (2012)
HIV-testing for key populations, pregnant women, ART for PMTCT and HIV-testing
for infants.
15. (2011) Area and Population: Health Management
Information System (HMIS) Township Profiles.
16. (2012) Administrative divisions: 2012 MIMU
P-Codes Release V (based on the 25 February 2011 Gazette issued by the Ministry
of Home Affairs — with UN/NGO field office updates on the number of villages).
17. (2009-2010) Poverty Incidence and Primary
School Net Enrolment Rate: Integrated Household Living Conditions Assessment (IHLCA).
18. Win S (2016) Poverty and child health. 3rd
Edn. J Myanmar Med Assoc, p: 17.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Rheumatology Research (ISSN:2641-6999)
- International Journal of Internal Medicine and Geriatrics (ISSN: 2689-7687)
- Chemotherapy Research Journal (ISSN:2642-0236)
- Journal of Nursing and Occupational Health (ISSN: 2640-0845)
- Journal of Ageing and Restorative Medicine (ISSN:2637-7403)
- Journal of Blood Transfusions and Diseases (ISSN:2641-4023)
- International Journal of Diabetes (ISSN: 2644-3031)